Peritonitis Caused by
Rupture of Infected Retroperitoneal Teratoma
Author: Yogesh Kumar Sarin
APSP J Case Rep 2012;
3: 2
Affiliation: Department of Pediatric Surgery Maulana
Azad Medical College New Delhi-110002, INDIA
Address for Correspondence: Prof. Yogesh Kumar Sarin, Head, Department
of Pediatric Surgery, Maulana Azad Medical College, Bahadur
Shah Zafar Marg, New
Delhi-110002, INDIA
Email: sarinyk@yahoo.com
Submitted on: 02-01-2012
Accepted on: 12-01-2012
Citation: Sarin YK. Peritonitis caused by rupture of infected
retroperitoneal teratoma. APSP J Case Rep 2012; 3: 2
Abstract
Retroperitoneal teratomas are usually asymptomatic,
though there have been isolated reports of retroperitoneal
teratomas presenting as intra-abdominal abscesses and peritonitis in adults. A 7-year-old girl who had presented with acute abdomen due to ruptured
retroperitoneal teratoma is reported.
Keywords: Retroperitoneal
teratoma, Peritonitis, Infected teratoma, Mature
teratoma.
Introduction
Retroperitoneal teratomas (RPTs) are uncommon tumors
representing about 5% of all teratomas [1]. Majority of them are benign. They
are typically asymptomatic; but when symptoms do occur due to enormity of their
size, patients will present with only abdominal distension or a palpable mass
on physical examination [2]. RPTs resulting in chemical peritonitis or
localized abscess and presenting as acute abdomen have rarely been described in
adults [3-6]. RPT presenting as acute abdomen has been even rarer in pediatric
patients. An extensive literature search could reveal only 2 cases hitherto [7,8]. We report here another case of ruptured retroperitoneal
teratoma that resulted in chemical peritonitis.
Case report
A
7-year-old girl presented with abdominal mass that was noted at birth. She had
abdominal pain and recurrent febrile episodes for the last 6 months that had
worsened a week before presentation. On examination, she was febrile with generalized
abdominal tenderness. A large well-defined, firm, fixed, tender mass, having
bosselated surface and measuring 15 cms in diameter occupied
entire left half of her abdomen. The fingers could be insinuated between the
mass and left costal margin above and the mass and the pelvic brim below. Leukocyte
count was 14,000/ mm3. Biochemical parameters were normal. Abdominal
roentgenogram showed a soft tissue shadow occupying the left half of the
abdomen displacing the stomach up and the bowel loops to the right. There were
extensive areas of calcification (Fig. 1). Chest x ray was normal. Abdominal
ultrasound revealed a large heterogeneous retroperitoneal mass pushing the left
kidney and the ureter with mild to moderate left hydronephrosis. CT scan
abdomen showed a well-defined retroperitoneal mass measuring 14cm x 10cm x 9cm in
the left half of the abdomen having mixed density, septations, calcifications
and teeth-like structures (Fig. 2,3). The mass displaced
the left kidney posteriorly and cranially, the sigmoid colon anteriorly, and aorta
and inferior vena cava to the right. The serum alpha fetoprotein levels were
within normal range. The diagnosis of infected retroperitoneal benign teratoma
was made.

Figure 1: Abdominal
roentgenograms showing soft-tissue mass displacing gut and having
calcifications.
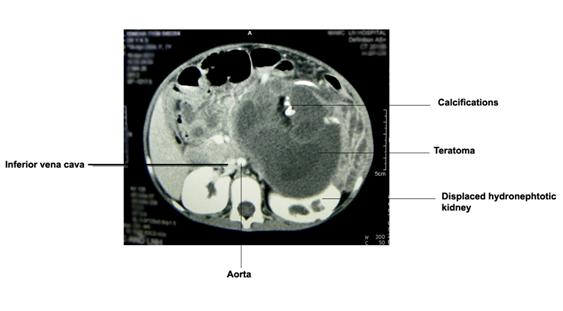
Figure 2: Abdominal
CT scan showing well circumscribed mass occupying left half of the abdomen,
having septations and calcifications and displacement of gut and major vessels.
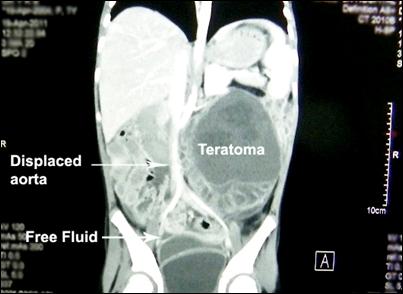
Figure 3: Abdominal
CT scan showing well circumcised mass occupying left half of the abdomen,
having septations and calcifications and displacing gut and major vessels.
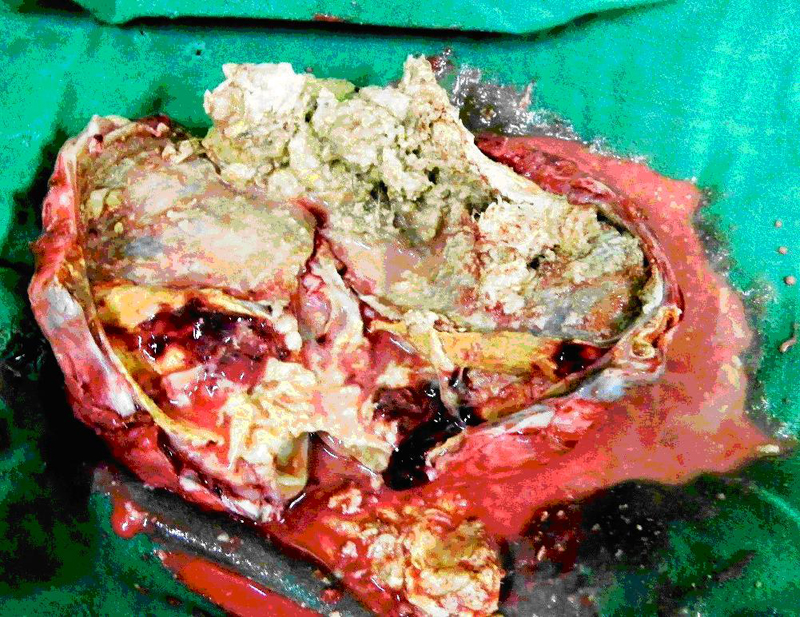
Figure
4: Excised specimen showing calcification, hair and other features suggestive
of mature teratoma.
At operation a small amount of thick turbid came out.
There were inter-loop pockets. The thick capsule of the tumor was found breached
at 2 places. The overlying sigmoid colon was firmly adherent to the tumor
capsule. The aorta, inferior vena cava and the mesenteric vessels were pushed
to the right and did not pose any risk to the dissection. Both ovaries were
normal
Excision of the large tumor necessitated resection and
anastomosis of the sigmoid colon. Though the tumor could be removed in toto, there was gross spillage intra-operatively. Few para-aortic lymph nodes were sampled. The resected specimen
had variegated appearance and there was evidence of cartilage, teeth, and hairs
(Fig. 4).
The patient did well post-operatively and was discharged on
15th postoperative day. The biopsy was reported as mature cystic
teratoma (dermoid cyst) with evidence of extensive xanthogranulomatous
reaction to keratin. The para-aortic lymph nodes had
only reactive changes. She has been on close follow up since last 6 months and
has been doing well.
Discussion
Retroperitoneal teratomas are rare,
representing only 1% to 11% of primary retroperitoneal neoplasms [8]. They
typically present as asymptomatic abdominal mass but can grow to enormous size.
There are only 2 children reported hitherto who had presented with acute
abdomen. Pontinen et al almost half century ago, had reported a retroperitoneal teratoma in a three year
old girl that simulated an acute appendicitis [7]. Nguyen et al had recently
described a 9-year-old girl who presented with an acute abdomen because of an
abdominal abscess that was treated with surgical drainage and antibiotics [8].
Fifteen years later, she had a recurrence of symptoms and the abscess was
ultimately recognized to be an infected retroperitoneal teratoma. Though the
diagnosis of infected retroperitoneal teratoma was made at the age of 24 years,
this teratoma must have been present since birth and got missed at the earlier
presentation in the childhood.
Most of the retroperitoneal tumors in childhood
are cystic and benign [2]. Spontaneous rupture of cystic retroperitoneal
teratomas is a rare occurrence probably because of the thick encasing
capsule. Taking analogy from cystic ovarian teratomas, two clinical
presentations could be associated with such intraperitoneal rupture
of benign cystic teratomas [9]. The first is acute peritonitis
caused by the sudden rupture of tumor contents, which may occur
spontaneously or more commonly in association with torsion, trauma,
infection, or labour. The second
presentation is chronic granulomatous peritonitis resulting from a
chronically leaking dermoid, which can be characterized by multiple
small white peritoneal implants, dense adhesions, and variable ascitis that simulate carcinomatosis or tuberculous peritonitis.
The latter is the more common presentation in case of cystic ovarian teratomas
[9].
CT scan is considered as better
radiological investigation than ultrasonography for the diagnosis of RPTs [10].
MRI has been also used recently. At CT, a mature RPT manifests as a complex
mass containing a well-circumscribed fluid component, adipose tissue, and
calcification [10]. The presence of hypoattenuating fat within the cyst and the
presence of calcifications in the cyst wall are considered highly suggestive of
cystic RPT [10]. At CT, the presence of fat-fluid levels in the peritoneum has
been quoted as a reliable sign of intraperitoneal rupture of abdominal teratoma
and subsequent chemical peritonitis [3]. However, the diagnosis of rupture of
RPT is usually made at operation.
The operative
management of RPTs, especially those with rupture, may be complex and
challenging. Despite their benign nature, the lesions can attenuate and
surround major vessels, making resection difficult. Preoperative
imaging has been known to be offer limited help in demonstrating the position
of the major vessels [11]. In particular, the veins may be effaced. Excision of
ruptured RPT in our case was also a formidable surgical exercise.
In conclusion, rupture of RPT is an extremely rare
phenomenon. It may be difficult to make a preoperative diagnosis and the
surgical excision could be a challenging task.
References
- Grosfeld JL, Ballantine TV, Lowe D, Baehner
RL. Benign and malignant teratomas in children: Analysis of 85 patients.
Surgery 1976; 80: 297-305.
- Chaudhary A, Misra
S, Wakhlu A, Tandon
RK, Wakhlu AK. Retroperitoneal teratomas in
children. Indian J Pediatr 2006; 73: 221-3.
- Ferrero A, Cacspedes
M, Cantarero JM, Arenas A, Pamplona M. Peritonitis due to
rupture of retroperitoneal teratoma: computed tomography diagnosis. Gastrointest Radiol 1990; 15:
251-2.
- Talwar N, Andley
M, Ravi B, Kumar A. Subhepatic abscess in
pregnancy- an unusual presentation of infected primary retroperitoneal
teratoma. Acta Obstet Gynecol Scand 2005; 84: 1127-8.
- Pandya JS, Pai MV, Muchhala S.
Retroperitoneal teratoma presenting as acute abdomen in an elderly person.
Indian J Gastroenterol 2000; 19: 89-90.
- Li
F, Munireddy S, Jiang L, Cheng N, Mao H, Pawlik TM. Infected primary retroperitoneal teratoma
presenting as a subhepatic abscess in a
postpartum woman. Am J Surg 2010; 199: e27-8.
- Pontinen PJ, Taulaniemi E. Retroperitoneal teratoma simulating an
acute appendicitis in a three year old girl. Ann Chir
Gynaecol Fenn 1962; 51:
244-6.
- Nguyen
CT, Kratovil T, Edwards MJ. Retroperitoneal
teratoma presenting as an abscess in childhood. J Pediatr Surg 2007; 42: E21-3.
- Pantoja E, Noy
MA, Axtmayer RW, Colon FE, Pelegrina
I. Ovarian
dermoids and their complications: comprehensive
historical review. Obstet Gynecol
Surg 1975; 30: 1-20.
- Jeffrey
RB Jr. Imaging of the peritoneal cavity. Curr Opin Radiol 1991; 3: 471-3.
- Jones NM, Kiely EM. Retroperitoneal
teratomas-potential for surgical misadventure. J Pediatr Surg 2008; 43: 184-6.