Early Recognition of H-Type Tracheoesophageal
Fistula
Authors: Muhammad Riazulhaq, Elbagir Elhassan
APSP J Case Rep
2012; 3: 4
Affiliation: Department of
Pediatric Surgery King Faisal Hospital, Taif, KSA
Address
for Correspondence: Dr. Muhammad Riazulhaq, Pediatric Surgeon, King Faisal Hospital
P.O Box 7390, Taif, KSA.
Email: riaz_rao@hotmail.com
Submitted
on: 24-12-2011
Accepted
on: 20-01-2012
Citation: Riazulhaq M,
Elhassan E. Early recognition of H-type tracheoesophageal
fistula. APSP J Case Rep 2012; 3: 4
Abstract
Tracheoesophageal fistula
(TEF) without associated esophageal atresia (EA) is a rare congenital anomaly.
Diagnosis in neonatal period is usually not made and most of the patients are
treated as cases of pneumonia. A case of H-type of tracheoesophageal fistula,
diagnosed within 24 hours of delivery based upon choking and cyanosis on first
trial of feed, is being reported. Diagnosis was confirmed with contrast
esophagram. Through cervical approach fistula was repaired and baby had
uneventful post operative outcome.
Keywords: Tracheoesophageal fistula, H-Type, Esophagus,
Atresia.
Introduction
H-type
TEF accounts for 4-5% of all congenital tracheoesophageal malformations. The clinical features
are variable; common being the recurrent respiratory symptoms, aspiration during
feeding with cyanosis, and abdominal distension. The early diagnosis of this
disorder is difficult and some cases may remain undiagnosed until late in
infancy or childhood. The first surgical repair of such a defect was
reported by Imperatori in 1939 [1-3]. We are reporting a case of H-type TEF that
was diagnosed within 24 hours of birth.
Case Report
A term male baby weighing 2.6 kg, born through normal vaginal
delivery with good APGAR scores was kept in nursery for observation. As a
routine, nasogastric tube was passed without any difficulty. On trial of first
feed baby developed choking and cyanosis. The systemic examination was essentially
unremarkable. With high suspicion of H-type TEF, a tube esophagram was
performed which showed contrast flowing into tracheobronchial tree through a
fistula between trachea and esophagus at the level of T1 (Fig.1,2).

Figure 1: Tube esophagram showing a
contrast within the tracheobronchial tree suggestive of TEF.
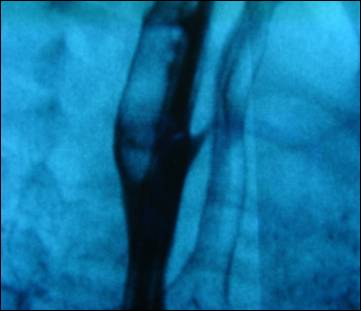
Figure 2: Negative macro image of
esophagram delineating fistula between trachea and esophagus
Oral feed was withheld and baby placed in semi upright position.
Intravenous fluids and antibiotics were started. Complete blood count,
coagulation profiles and blood chemistry were in normal range. Ultrasound
abdomen was unremarkable while echocardiogram showed a small patent ductus arteriosus (PDA). Patient
was operated through right low transcervical approach at 36-hour age. Thyroid
and cervical trachea were exposed; division of thyroid veins, upward
displacement of right lobe of thyroid and lateral displacement of trachea
exposed the fistula. Recurrent laryngeal nerve was identified and preserved.
Fistula was divided and repaired. After surgery patient was kept on elective
ventilation for 72 hours. Nasogastric feed was started on 4th post
operative day. Contrast esophagram
showed no leakage. Patient was discharged on 10th day of operation
after establishing oral feeding.
Discussion
Most
infants with EA with TEF have proximal atresia with distal TEF. They are easily
diagnosed soon after birth as to apparent clinical features, nevertheless
H-type TEF are not diagnose early because esophagus is patent. Many diagnostic methods have been advocated for the diagnosis of
H-type fistula. Esophagram is usually a reliable method to identify congenital
H-type tracheoesophageal fistula, though often difficult, requiring multiple attempts
before the defect is confirmed. Furthermore, contrast-enhanced studies have the
potential risk of aspiration pneumonia and pulmonary injury and should be
performed with adequate neonatal emergency resuscitation at hand. Endoscopic
methods like bronchoscopy and esophagoscopy have the advantage of being
diagnostic allowing placement of a catheter across the fistula to
assist in its localization during surgery [2-4]. H-type
TEF is associated with other malformations in about 30% of cases, including
VACTERL/VATER, CHARGE syndrome, Goldenhar’s syndrome, esophageal stenosis, and
syndactyly [5]. The index case has none of these associations.
Different surgical approaches have been
described for this anomaly. For proximally located fistula the approach of
choice is cervicotomy and in cases of distal fistula thoracotomy is usually
preferred. Biechlin et al reported a series of 8
cases of H-type TEF, all were repaired through right cervicotomy. An
alternative thoracoscopic approach in a newborn has
recently been reported by Allal et al. Surgery consists of ligation and division of the fistula and
repair of the tracheal and esophageal walls. Brookes et al reported seven patients of H-type
TEF and one patient with a missed proximal H-type fistula associated with
esophageal atresia. They presented with coughing while feeding, recurrent
pneumonia, and episodic cyanosis. A delay in diagnosis was seen in 4 patients
and ranged from 2.5 months to 5.9 years. In all patients, the diagnosis was
made on esophagram. The level of the fistulae was between C5 and T3, and all
were successfully repaired via a right cervical approach [6-9].
In present case cervical approach was chosen with
preservation of recurrent laryngeal nerve. The outcome in present case was
satisfactory as baby discharged home on 10th POD in stable
condition. A high index of suspicion in cases of cyanosis and choking on first
feed and recurrent respiratory symptoms even when esophagus is patent, indicate
H-type TEF until proved otherwise. Such patients must be thoroughly
investigated to demonstrate the anomaly.
References
1. Chueh H, Kim MJ, Jung JA. A case of acute
respiratory distress syndrome associated with congenital H-type
tracheoesophageal fistula and gastroesophageal reflux. Korean
J Pediatr 2008; 51:892-5.
2. Nq J, Antao B, Bartram J, Raqhavan A, Shawis R. Diagnostic difficulties in the management of
H-type tracheoesophageal fistula. Acta Radiol 2006;47:801-5.
3. Imperatori
CJ. Congenital tracheo-esophageal fistula without atresia
of the esophagus Arch Otolaryngol 1939;30:352.
4. Karnak I, Senocak ME, Hicsonmez A, Buyukpamukcu N. The diagnosis and treatment of H-Type
tracheoesophageal fistula. J Pediatr Surg 1997;32:1670-4.
5. Genty E, Attal
P, Nicollas R, Roger G, Triglia
JM, Garabedian EN, Bobin S.
Congenital tracheoesophageal fistula
without esophageal atresia. Int J Pediatr
Otorhinolaryngol 1999;48:
231-8.
6. Crabbe D. Isolated tracheo-oesophageal
fistula. Pediatr Respir Rev
2003;4:74-8.
7.
Biechlin A, Delattre A, Fayoux P.
Isolated congenital tracheoesophageal fistula. Retrospective analysis of 8
cases and review of the literature. Rev
Laryngol Otol Rhinol
2008;129:147-52.
8. Allal H, Montes-Tapia F, Andina G. Thoracoscopic repair of H-type tracheoesophageal fistula in the
newborn: a technical case report. J Pediatr Surg 2004;39:1568-70.
9. Brookes JT, Smith MC,
Smith RJ,
Bauman NM,
Manaligod JM, Sandler AD. H-type congenital tracheoesophageal fistula:
University Of Iowa experience 1985 to 2005. Ann Otol Rhinol laryngol 2007;116:363-8.