Spontaneous Intracerebral Haemorrhage in a Child
Authors: Amit Agrawal,1 Vikram Jeet Singh Dhingra2
APSP J Case Rep 2012; 3: 3
Affiliation: Department of
Neurosurgery1 and Surgery,2
MM Institute of Medical Sciences & Research, Mullana (Ambala), India.
Address for Correspondence: Dr Amit Agrawal MM
Institute of Medical Sciences & Research Mullana (Ambala) 133203 Haryana, India.
Email: dramitagrawal@gmail.com
Received on: 30-10-2011
Accepted on: 15-11-2011
Citation: Agrawal
A, Dhingra VJS. Spontaneous
intracerebral haemorrhage in a child. APSP J
Case Rep 2012; 3: 3
Abstract
Spontaneous
intracerebral haemorrhage (SICH) is a rare occurrence
in children, with different aetiological factors,
clinical characteristics and prognosis. A 14 year male child had sudden onset
of headache associated with multiple vomiting. Magnetic resonance imaging
showed deep seated intracerebral haematoma. Haematoma was evacuated
successfully and child recovered without deficits. A high index of suspicion is
necessary for the diagnosis of spontaneous intracerebral haemorrhage
in children.
Keywords: Spontaneous
intracerebral haemorrhage, Intracerebral
haematoma
Introduction
Spontaneous
intracerebral haemorrhage is a rarely reported in
children. Its aetiology is different from that of
adults and distinct clinical characteristics and prognosis. If not suspected
these cases can be misdiagnosed initially as meningitis or common cold [1-4]. Herein a case of SICH is presented to highlight recognition
of this condition.
Case report
A
14 year old male child had sudden onset of headache one and half month back
which was associated with multiple episodes of vomiting. He was treated at
local hospital and headache was reduced in intensity after oral analgesics.
There was no history of fever, seizures or focal neurological deficits. His
general and systemic examination was unremarkable. Higher mental functions were
normal and there was no focal neurological deficit. Fundus
showed bilateral early papilloedema. Blood
investigations were normal. He was investigated with magnetic resonance imaging
(MRI) which showed evidence of left basal ganglionic haematoma with mass effect
and midline shift (Fig. 1,2). He underwent left
frontal craniotomy and haematoma was approached through the middle frontal gyrus as it was approaching to the surface in that region.
There was thin capsule containing altered blood which was removed completely.
Histopathology showed organizing blood clot and there was no evidence of tumor
cells or any abnormal vessels (Fig. 3). Child is doing well and there are no
neurological deficits.

Figure 1: MRI
axial section showing well defined lesion in left basal ganglion with evidence
of haemorrhage, (A) T1, (B) T2, (C) FLAIR images and
(D) minimal enhancement after contrast administration.
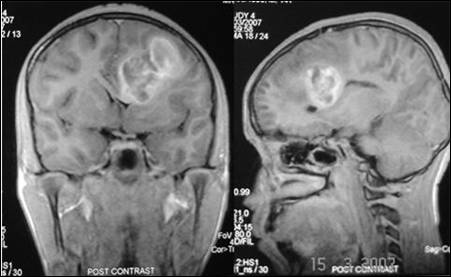
Figure 2: Contrast MRI coronal and sagittal sections
showing more details of the lesion; note the mass effect and distortion of
corpus callosum.
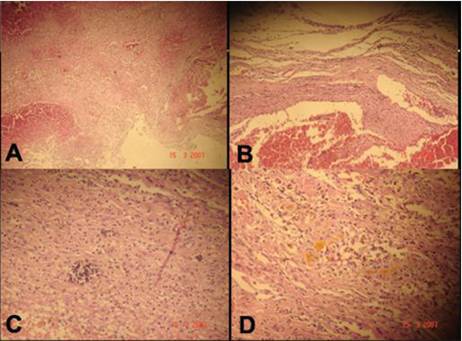
Figure 3: Photomicrograph showing features of organized
haematoma (A) 20x, (B) 40x, (C) evidence of calcification and (D) haemosiderin deposits.
Discussion
Spontaneous
intracerebral haemorrhage more commonly affects male
children. The leading cause of SICH is arteriovenous
malformation. Other causes include haematologic or
coagulation disorders, serious liver disorder due to alpha-l-antitrypsin
deficiency; bleeding from an undiagnosed tumor and sometime one may not be able
to find the aetiology. SICH usually present with a
sudden onset of headache that may be associated with vomiting and altered
consciousness. Magnetic resonance imaging scans is the most important
non-invasive modality for the investigation. Cerebral angiography can diagnose arteriovenous malformations. Laboratory examinations are
directed to rule out the other causes of bleeding i.e. bleeding disorders or haematological malignancies [1-4].
Management
of critical SICH consists in preventing or treating cerebral hypertension and
seizures. Prompt excision of the haematoma improves the outcome as in present
case. Patients with poor neurological status at the time of admission and SICH
located at brain stem, cerebellum, and multiple subcortical
areas have higher mortality rates. Intraparenchymatous
haematomas in children have a high mortality and many
sequelae. A high index of suspicion is necessary for
the diagnosis of spontaneous intracerebral haemorrhage
in children as the incidence of SICH is very low and presenting symptoms may be
non-specific [2-4].
References
- Al-Jarallah A, Al-Rifai MT, Riela AR, Roach ES. Nontraumatic
brain hemorrhage in children: etiology and presentation. J Child Neurol.
2000; 15:284-9.
- Lin CL, Loh JK, Kwan AL, Howng SL.
Spontaneous intracerebral hemorrhage in children. Kaohsiung J Med Sci.
1999; 15:146-51.
- Marzo-Sola
ME, Carod-Artal J, Garaizar
C, Prats-Vinas JM. Intraparenchymal
hematomas: specific features in children. Rev Neurol
1998; 26: 561-3.
- May Llanas ME, Alcover Bloch E, Cambra Lasaosa FJ, Campistol Plana J, Palomeque
Rico A. Non-traumatic cerebral hemorrhage in childhood: etiology, clinical
manifestations and management. An Esp
Pediatr 1999; 51: 257-61.