Omental Cake: A Radiological Diagnostic
Sign
Authors: Naima Zamir,* Jamshed Akhtar, Soofia Ahmed
APSP Journal of Case Reports 2011; volume 2 (3): 27
Address: Department of Paediatric Surgery National Institute of
Child Health, Rafiqui Shaheed Road Karachi 75510, Pakistan.
Date
of Submission: 23-07-11
Date
of Acceptance: 30-07-11
Citation: Zamir N, Akhtar J, Ahmed S. Omental cake: a radiological
diagnostic sign. APSP J Case Rep 2011;2:27
A ten-year old male child,
weighing 20 kg, was admitted through emergency with abdominal fullness and
pain. There was a history of sustaining
a trivial injury to abdomen two months back following which he developed mild
abdominal pain. Intensity of pain increased gradually and became unbearable,
along with abdominal distention. There was single episode of bleeding per rectum and off and on fever during this period with
no other associated symptoms like vomiting and constipation. Past medical and
family history was unremarkable.
Examination showed pale,
anxious, thin built child with heart rate 120/min, respiratory rate 24
breaths/min, and temperature 101° F. Abdomen was protuberant, firm and severely
tender. Digital rectal examination revealed a firm mass palpable on anterior aspect
of rectal wall with mobile overlying mucosa, finger stall stained with blood.
Despite the
history of trauma, signs and symptoms were more in favor of abdominal
tuberculosis, with the differential of post traumatic infected haematoma, and
sub acute or delayed presentation of infections like appendicitis and enteric
fever. His haemoglobin
was 7.8 g/dl, total leukocytes 14200/cmm, neutrophils 83%, ESR 10mm in 1st
hour. Ultrasound abdomen showed moderate amount of fluid in abdomino-pelvic
cavity. CT scan showed thick omentum, matted gut
loops with lymphadenopathy and fluid collection in the peritoneal cavity (Fig.
1,2).
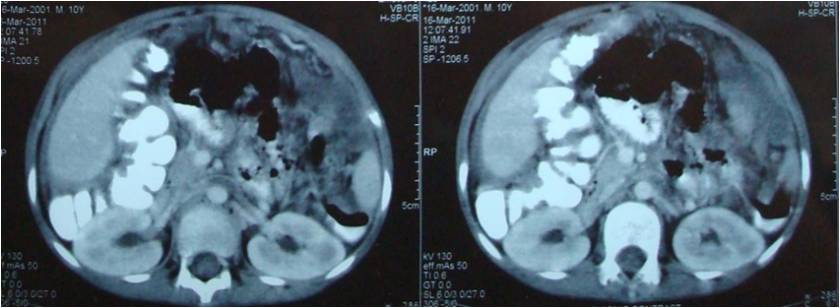
Figure 1: Thick omentum, matted gut loops
with ascitic fluid collection.
.

Figure 2 : Thick solid (cake) omentum pushing all the small bowel loops towards
right lower quadrant with encapsulation of the colon.
With the suspicion of tuberculosis anti tuberculous
therapy was started, but pain remained thus following optimization the patient
was explored. There was thickened, firm omentum occupying whole of abdomen
extending into the pelvis (omental cake), pushing small bowel to right lower
quadrant and densely encapsulating sigmoid colon with approximately 100cc of
clear yellow fluid in peritoneal cavity. An iatrogenic tear occurred in the
descending colon during dissection which revealed normal looking mucosa.
Debulking of the mass with end stoma at the descending colon and Hartmann’s
procedure of the distal gut were done. Biopsy of the sigmoid colon along with
the thickened omentum was sent for histopathology. Recovery was smooth and
patient discharged on 8th post operative day. Biopsy revealed
moderate to poorly differentiated mucinous adenocarcinoma infiltrating both
colon and omentum. Patient is currently registered with oncology department for
further evaluation and management.
Discussion
Omental spread of diseases
ranges from inflammation, infection, to malignancy. Malignancy can be either primary tumor of
omentum, or spread from the adjacent or remote areas. The different patterns of
omental involvement include seedlings, localized or diffuse infiltration of
omental fat by soft tissue density material. The resulting thickened solid omentum is called as omental caking [1].
Thick caking is an indicator
of advanced stage of any disease. It is often documented in adult population. Metastatic
peritoneal tumors most often originate from the ovary, stomach, pancreas,
colon, uterus, and bladder. Haematogenous metastases
from malignant melanoma, as well as breast and lung carcinoma, are also common.
In developing countries it is also found to
be associated with fibrotic type of peritoneal tuberculosis. In paediatric population it is uncommon though reported in
cases of rhabdomyosarcoma and lymphoma. Mucinous adenocarcinoma of colon itself
is a rare entity in paediatric population, and has an
aggressive course, but omental caking is infrequently reported with this type
of cancer [2-7].
Computed tomography is a good diagnostic
modality in cases of omental pathologies. In the normal anatomy, omentum looks
like bands of fatty tissue with some fine blood vessels while in cases of
ascites it appears as thin fatty layer. Soft deposits can appear as
seeding. Omental caking is actually a
radiological sign which on CT scan can be easily identified as diffuse
haziness, or a mass like effect. The ascitic fluid encased in the thickened omentum
appears as cystic spaces [3].
In
our patient CT scan showed, thickened omentum almost occupying the whole of
abdomen pushing the matted thick walled gut loops towards one side with ascites.
These findings are very much suggestive of advanced pathology especially
secondary to malignancy but since such pathology hardly documented in cases of paediatric population our provisional diagnosis was
tuberculosis. CT scan findings along with the relevant clinical and demographic
data can be of great help in making a diagnosis and also in planning the
management of the patients with omental pathology.
References
1. Cooper C, Jeffery RB, Silverman PM, Federle
MP, Chun GH. Computed tomography of omental pathology. J Comput
Assist Tomogr 1986;10:62-6.
2. Ejaz K, Raza S, Kashif W. Omental caking:
a rare but grave sign in prognosis of carcinoma endometrium.
J Surg Pakistan 2008;13:175-7.
3. Yoo E,
Kim JH, Kim M,Yu J, Chung J, Yoo
H, Kim KW. Greater and lesser omentum:
Normal anatomy and pathologic processes. Radiographics
2007;27:707-20.
4. Sharma MP, Bhatia V. Abdominal tuberculosis. Indian J Med
Res 2004;120:305-15.
5. Chung
CJ,
Bui
V,
Fordham
LA,
Hill
J,
Bulas D. Malignant intraperitoneal neoplasms of childhood. Pediatr Radiol 1998;28:317-21.
6. Zamir N, Ahmed S, Akhtar J. Mucinous adenocarcinoma of
colon. APSP J Case Rep 2010;1:20
7. Pickhardt PJ, Bhalla S. Primary neoplasms of peritoneal and sub-peritoneal origin: CT
findings. Radiographics 2005;25:983-95.